Discover how missed calls cost medical practices up to $500,000 annually in lost revenue. Learn the shocking financial impact of unanswered phones and proven solutions to capture every patient opportunity.

The silent revenue killer lurking in every medical practice isn't a billing error, insurance denial, or operational inefficiency—it's the phone calls that never get answered. While practice administrators focus on optimizing appointment schedules and reducing no-shows, a far more devastating financial hemorrhage occurs every time a patient call goes to voicemail during business hours.
Recent industry analysis reveals that the average medical practice loses between $200,000 and $500,000 annually from missed calls alone, with some high-volume specialty practices experiencing losses exceeding $1 million per year. These aren't theoretical calculations or worst-case scenarios—they represent the documented financial impact of inadequate phone coverage that affects thousands of medical practices across the United States.
The mathematics of missed call revenue loss is both straightforward and shocking. When a potential patient calls seeking care and receives no answer, that interaction represents far more than a simple missed connection. Each unanswered call potentially eliminates years of patient lifetime value, referral opportunities, and practice growth that compound over time into massive financial losses.
Understanding the true cost of missed calls requires examining the complete patient acquisition and retention ecosystem, from initial contact through long-term care relationships. Medical practices that implement comprehensive call answering solutions typically recover 60-80% of previously lost revenue within the first year, demonstrating the immediate and substantial return on investment available through professional phone coverage.
Daily Call Volume and Miss Rate Analysis
The foundation of missed call revenue calculations begins with understanding typical call patterns in medical practices. A standard five-physician primary care practice receives approximately 150-200 calls per day, with peak volumes occurring between 8:00-10:00 AM and 1:00-3:00 PM when patients schedule appointments and seek urgent care guidance.
During these peak periods, practices with inadequate phone staffing miss 15-30% of incoming calls, translating to 25-60 missed opportunities daily. Even practices with dedicated front desk staff experience significant miss rates when employees handle multiple responsibilities, including patient check-in, insurance verification, and administrative tasks that prevent immediate phone response.
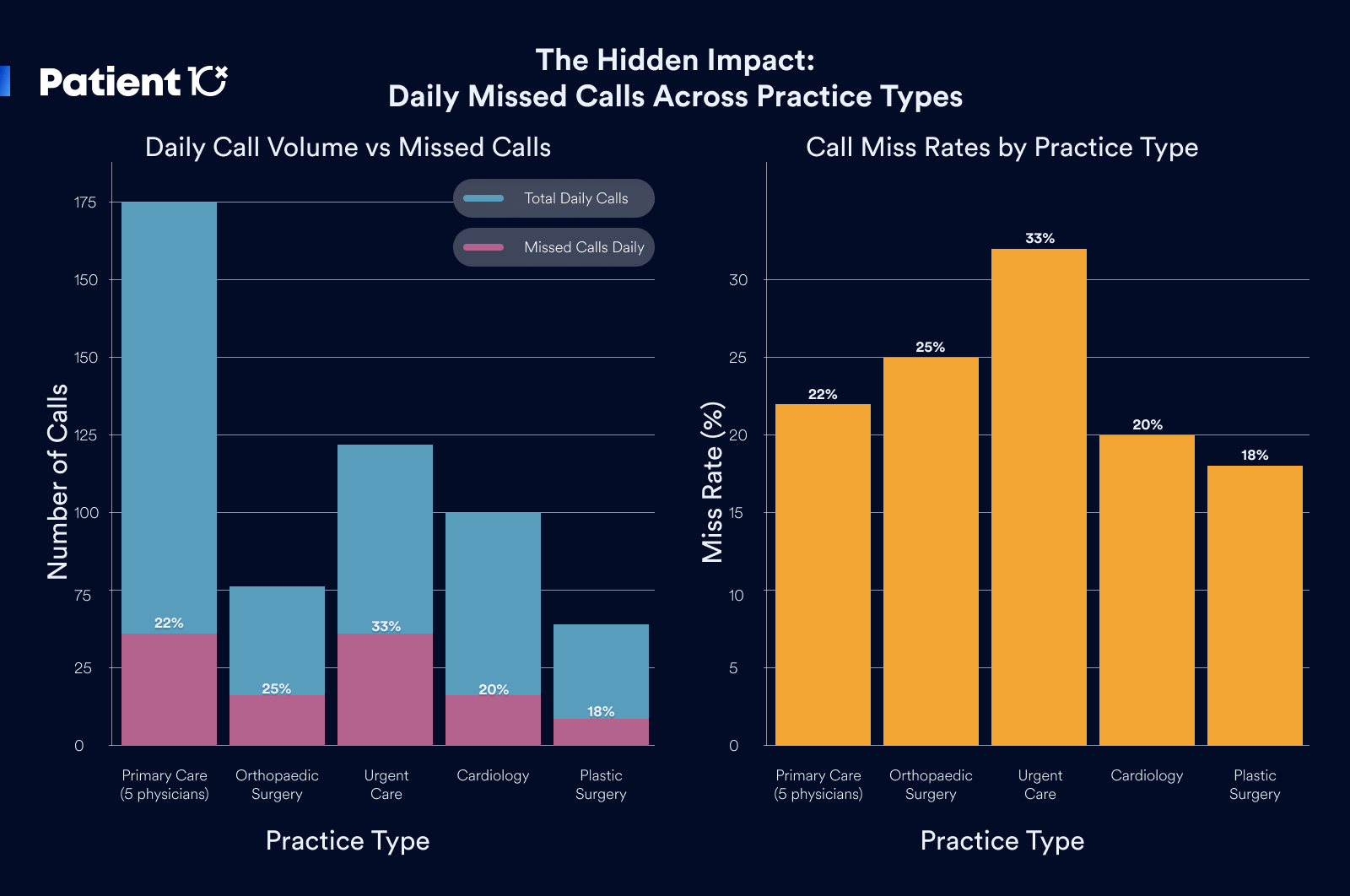
The compounding effect of missed calls becomes apparent when examining weekly and monthly patterns. A practice missing just 30 calls per day accumulates 150 missed opportunities weekly, 650 monthly, and approximately 7,800 annually. Each missed call represents a potential patient seeking care, with conversion rates from answered calls to scheduled appointments ranging from 25-40% depending on specialty and urgency of need.
Patient Lifetime Value Calculations by Specialty
The financial impact of missed calls varies dramatically by medical specialty, with patient lifetime values ranging from $2,000 for basic primary care to over $50,000 for complex surgical specialties. Primary care patients typically generate $3,000-$5,000 in lifetime revenue through regular visits, preventive care, and chronic condition management over a 5-10 year relationship.
Specialty practices experience significantly higher patient lifetime values due to complex procedures, ongoing treatment protocols, and referral relationships. Cardiology patients average $8,000-$15,000 in lifetime value, while surgical specialties, including orthopedics and plastic surgery, can generate $20,000-$50,000 per patient through procedures, follow-up care, and revision surgeries.
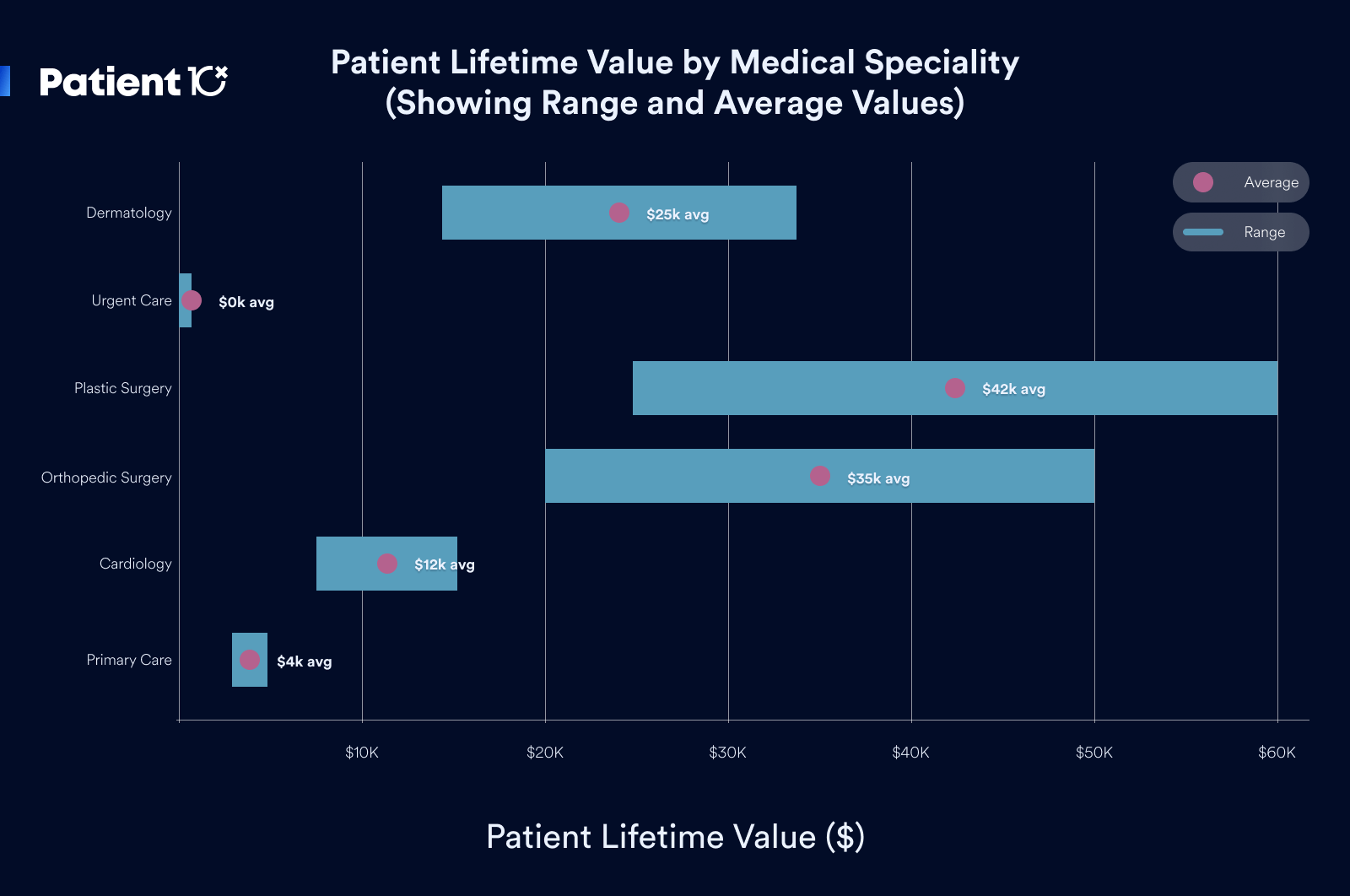
Emergency and urgent care practices operate on different models with lower individual visit values but higher volume potential. Each missed call in urgent care represents immediate revenue loss of $200-$500 per visit, with limited opportunity for relationship development but significant volume impact during peak illness seasons.
Annual Revenue Loss Calculations
Conservative calculations for a typical five-physician primary care practice demonstrate the massive financial impact of missed calls. Assuming 30 missed calls daily with a 30% conversion rate to appointments, the practice loses 9 potential patients per day. With an average patient lifetime value of $4,000, daily revenue loss equals $36,000, translating to $180,000 weekly and $9.36 million annually.
However, these calculations represent gross potential rather than net loss, as practices typically operate at 80-90% capacity during peak periods. Realistic revenue loss calculations must account for scheduling availability, with missed calls during fully booked periods representing future opportunity loss rather than immediate revenue impact.
More accurate analysis suggests that practices lose 40-60% of missed call potential revenue, accounting for scheduling constraints and patient urgency factors. This adjustment reduces the annual loss calculation to $3.7-$5.6 million in gross potential, with net revenue loss of $200,000-$500,000 annually for a typical primary care practice.
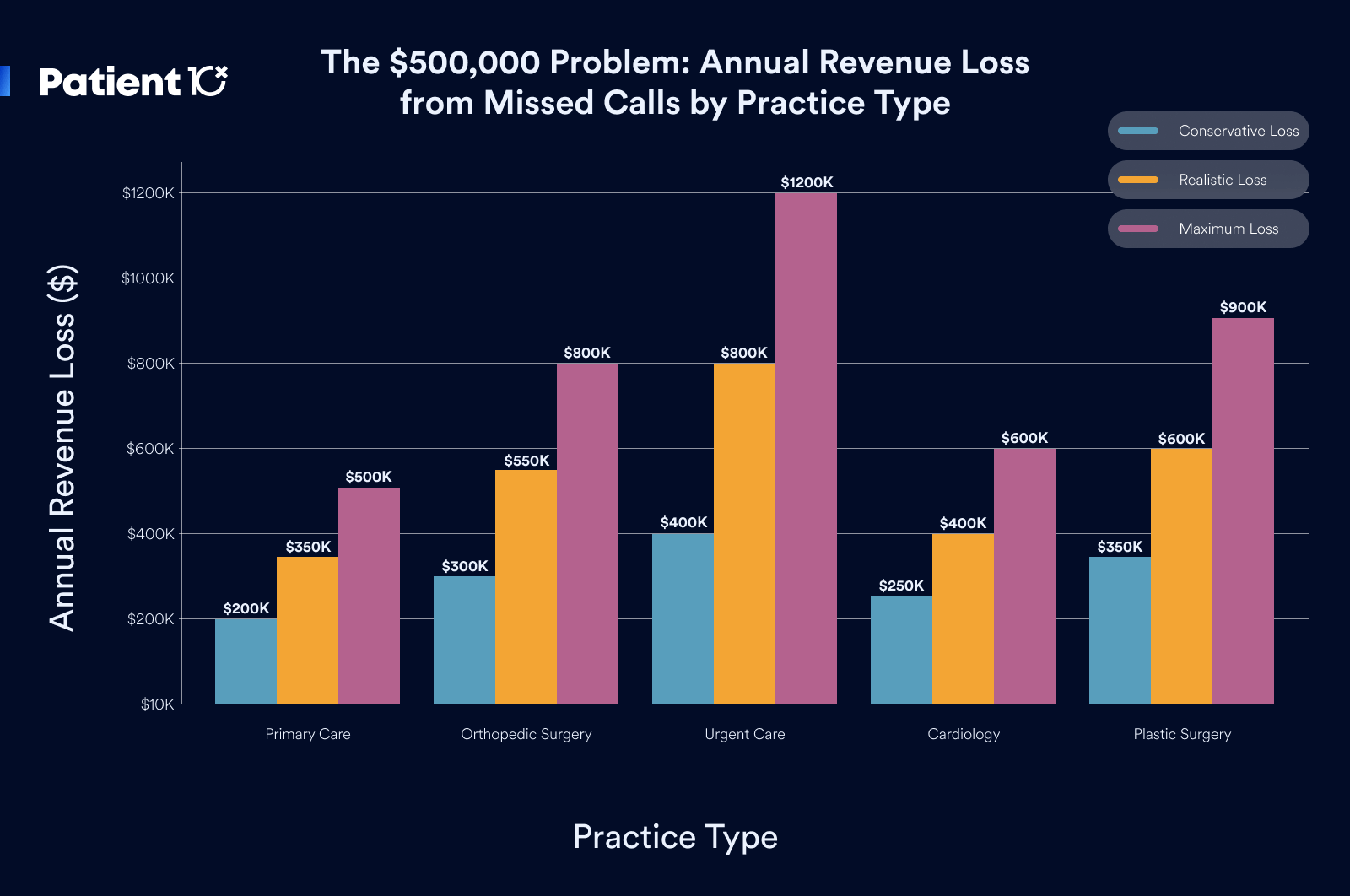
Specialty Practice Revenue Impact Analysis
Surgical and specialty practices experience disproportionately higher revenue loss from missed calls due to elevated patient lifetime values and referral relationship complexity. A busy orthopedic surgery practice missing 20 calls daily with a 25% conversion rate loses 5 potential patients worth $25,000 each in lifetime value, representing $125,000 in daily gross potential or $45.6 million annually.
Accounting for scheduling constraints and procedure availability, orthopedic practices typically lose $300,000-$800,000 annually from missed calls. Plastic surgery and dermatology practices with elective procedure focus experience similar losses, as missed calls often represent patients seeking consultations for high-value cosmetic or reconstructive procedures.
Emergency medicine and urgent care practices face unique challenges with missed calls representing immediate revenue loss without future opportunity for recovery. A busy urgent care center missing 40 calls daily during peak periods loses $8,000-$20,000 in immediate revenue, translating to $2.9-$7.3 million annually in gross potential and $400,000-$1.2 million in realistic net loss.
Referral Network Disruption
The financial impact of missed calls extends far beyond individual patient loss through disruption of referral networks that represent the foundation of specialty practice growth. When referring physicians cannot reach specialists for urgent consultations or patient transfers, they develop alternative referral patterns that permanently redirect patient flow to competing practices.
Each missed referral call potentially eliminates not just the immediate patient but the entire future referral relationship with the referring physician. Primary care physicians who experience difficulty reaching specialists for consultations or urgent transfers quickly establish relationships with more accessible practices, creating permanent revenue loss that compounds over years.
The mathematics of referral loss demonstrates a devastating long-term impact. A cardiologist who loses referral relationships with three primary care physicians due to poor phone accessibility may forfeit 200-300 annual referrals worth $2-3 million in lifetime patient value. This referral disruption often proves irreversible, as referring physicians rarely return to specialists who previously demonstrated poor accessibility.
Online Reputation and Review Impact
Missed calls increasingly translate into negative online reviews that damage practice reputation and reduce future patient acquisition effectiveness. Patients who cannot reach practices during urgent situations frequently express frustration through Google reviews, Yelp comments, and social media posts that influence thousands of potential patients.
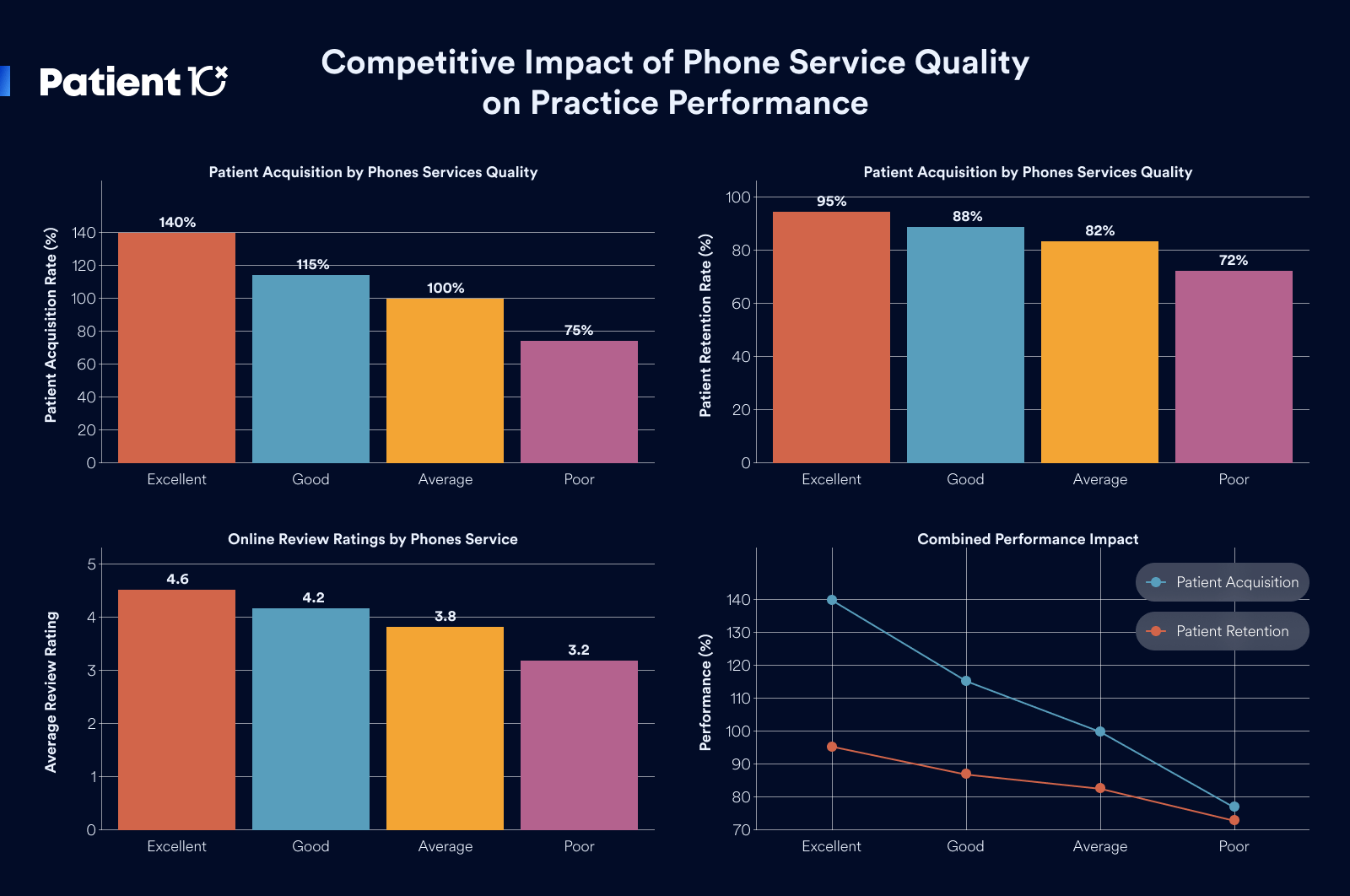
Analysis of online reviews for medical practices reveals that phone accessibility ranks among the top three factors influencing patient satisfaction scores. Practices with poor phone responsiveness average 3.2-3.8 stars across review platforms, while those with excellent phone service achieve 4.3-4.7 star ratings that significantly improve search visibility and patient acquisition.
The financial impact of reputation damage compounds over time as negative reviews reduce organic patient acquisition and increase marketing costs required to overcome poor online presence. Practices with below-average review scores typically experience 20-30% higher patient acquisition costs and 15-25% lower conversion rates from marketing campaigns.
Patient Loyalty and Retention Erosion
Existing patients who experience difficulty reaching their practice during urgent situations often begin exploring alternative providers, leading to gradual patient base erosion that reduces practice stability and predictable revenue. Long-term patients who cannot access their physicians during emergencies frequently transfer care permanently to more accessible practices.
The lifetime value impact of patient defection extends beyond individual patient loss to include family members and social network referrals that typically accompany satisfied patients. A family practice losing a satisfied patient family due to poor phone accessibility may forfeit $15,000-$25,000 in immediate lifetime value, plus 5-10 additional referrals worth $50,000-$100,000 in extended network value.
Patient retention analysis demonstrates that practices with excellent phone accessibility maintain 85-95% annual patient retention rates, while those with poor phone service experience 70-80% retention. This 10-15% retention difference translates to a massive revenue impact over time as practices must continuously acquire new patients to replace those lost through accessibility failures.
Call Response Standards and Patient Expectations
Healthcare industry standards for phone response have evolved significantly with patient expectations now demanding immediate accessibility during business hours. Current benchmarks suggest that medical practices should answer 90% of calls within three rings, with maximum hold times not exceeding two minutes for non-emergency situations.
Patient survey data reveals that 67% of healthcare consumers will call alternative providers if their primary practice doesn't answer within three rings, while 85% expect calls to be answered during posted business hours without exception. These expectations reflect broader customer service standards from other industries that have influenced healthcare consumer behavior.
Competitive analysis of high-performing medical practices demonstrates that superior phone accessibility serves as a primary differentiator in crowded healthcare markets. Practices that consistently answer calls promptly experience 25-40% higher patient acquisition rates and 15-20% better patient retention compared to competitors with poor phone service.
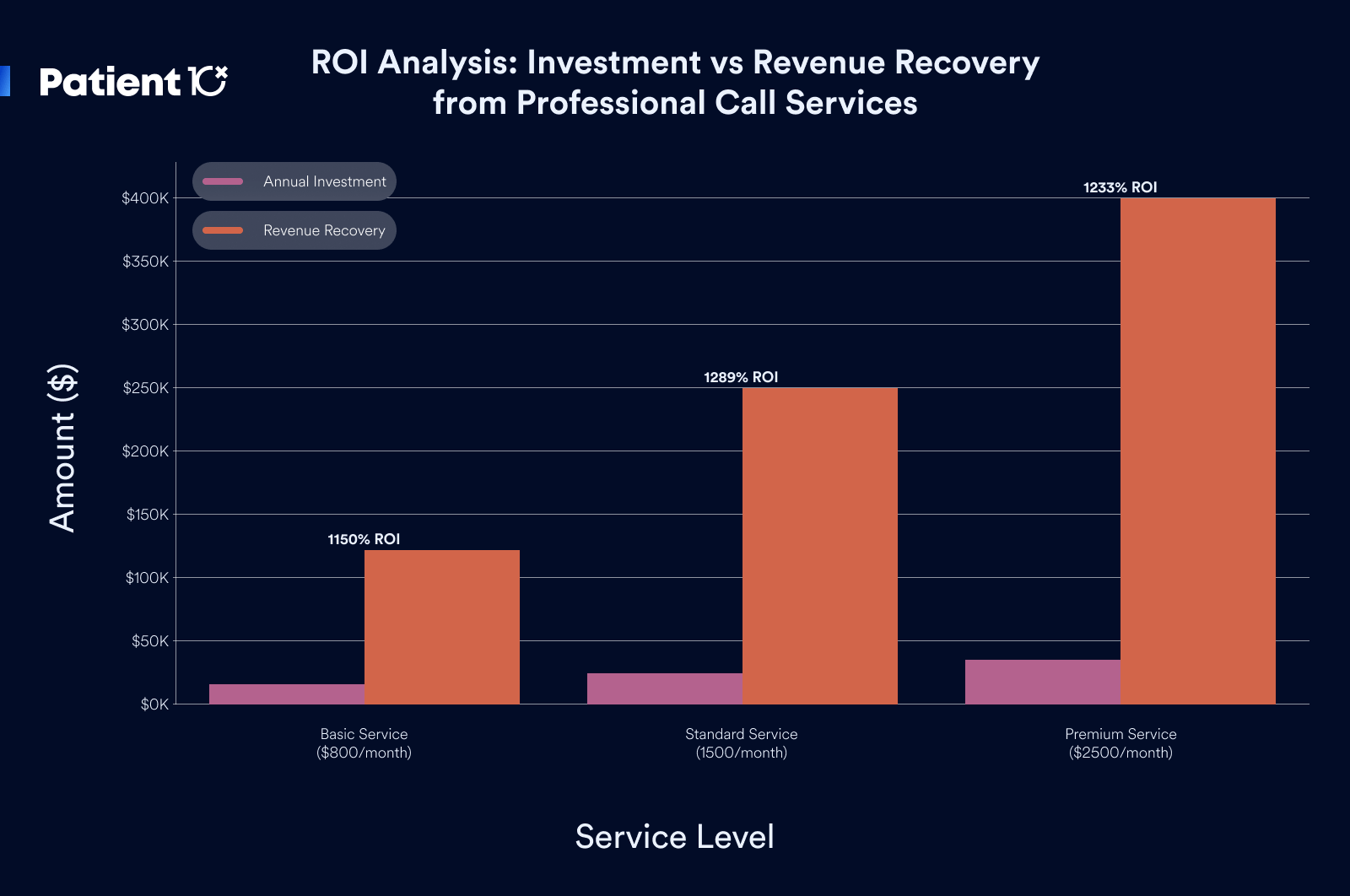
Technology Solutions and Implementation Costs
Modern call answering solutions for medical practices range from basic voicemail systems to comprehensive live answering services with full integration capabilities. Basic automated systems cost $50-$200 monthly but provide limited patient satisfaction and no revenue capture from missed calls.
Professional live answering services specifically designed for healthcare practices typically cost $800-$2,500 monthly, depending on call volume and service level requirements. These services provide HIPAA-compliant call handling, appointment scheduling integration, and emergency escalation protocols that capture revenue while maintaining patient satisfaction.
The return on investment for professional call answering services typically ranges from 300-800% annually when accounting for captured revenue, improved patient satisfaction, and reduced staff stress. Practices implementing comprehensive call solutions usually recover their investment within 2-4 months through increased patient acquisition and retention.
Market Positioning and Competitive Advantage
Medical practices that establish superior phone accessibility as a core service differentiator often capture significant market share from competitors with poor phone service. This competitive advantage becomes particularly pronounced during healthcare crises or seasonal demand spikes when patients prioritize accessibility over other factors.
The marketing value of excellent phone service extends beyond immediate patient acquisition to include word-of-mouth referrals, positive online reviews, and an enhanced reputation that reduces overall marketing costs. Practices known for superior accessibility often achieve 20-30% lower patient acquisition costs compared to competitors relying solely on traditional marketing approaches.
Long-term competitive positioning through phone service excellence creates sustainable advantages that prove difficult for competitors to replicate quickly. Establishing a reputation for accessibility requires consistent performance over months or years, providing first-mover advantages for practices that prioritize comprehensive call management solutions.
Professional Call Answering Service Integration
The most effective solution for capturing missed call revenue involves partnering with professional medical call answering services that provide seamless integration with existing practice management systems. These services employ trained healthcare professionals who understand medical terminology, HIPAA requirements, and emergency protocols essential for maintaining patient safety and satisfaction.
Professional services typically offer 24/7 coverage including after-hours emergency triage, appointment scheduling integration, and real-time message delivery to physicians and staff. The investment in professional call answering usually ranges from $1,000-$3,000 monthly for comprehensive coverage, representing a fraction of the revenue typically lost through missed calls.
Implementation of professional call answering services usually requires 2-4 weeks for complete integration, including staff training, protocol development, and system testing. Most practices experience immediate improvement in call response rates and patient satisfaction, with revenue impact becoming apparent within 30-60 days of implementation.
Staff Training and Internal Process Optimization
Practices preferring internal solutions can significantly improve call response through comprehensive staff training and process optimization focused on phone prioritization and efficiency. This approach requires dedicated investment in training, scheduling adjustments, and performance monitoring to achieve sustainable improvement.
Effective internal solutions typically involve hiring dedicated phone staff, implementing call routing systems, and establishing clear protocols for call prioritization and escalation. The total cost for internal improvements usually ranges from $40,000-$80,000 annually including salary, benefits, and system costs.
While internal solutions provide greater control over call handling, they require ongoing management and typically achieve lower performance levels compared to professional services. Most practices find that hybrid approaches combining internal staff with professional overflow coverage provide optimal results and cost-effectiveness.
Technology Integration and Automation Solutions
Advanced technology solutions, including AI-powered call routing, automated appointment scheduling, and intelligent message prioritization, can significantly improve call handling efficiency while reducing staff workload. These systems typically integrate with existing practice management platforms to provide seamless workflow enhancement.
Modern call management technology costs range from $200-$1,000 monthly, depending on features and integration complexity. While technology solutions improve efficiency, they cannot fully replace human interaction required for complex patient needs and emergency situations.
The most effective approach typically combines technology automation for routine calls with professional human support for complex situations and overflow coverage. This hybrid model maximizes efficiency while ensuring patient satisfaction and revenue capture across all call types and volume levels.
Patient10x's call answering services have helped medical practices across the country capture millions in previously lost revenue while improving patient satisfaction and reducing staff stress. To learn more about how Patient10x can help your practice eliminate missed call revenue loss, visit Patient10x.com or contact our team for a comprehensive practice analysis and revenue recovery consultation.